Knowledge, perception and preparedness of future prescribers about antimicrobial stewardship
Abstract
The study was aimed to evaluate the knowledge, perception and preparedness of the 4th year students of three medical colleges of Bangladesh during January 2016. The questionnaire was designed to evaluate knowledge, perception and preparedness about antimicrobial stewardship and resistance. Out of two hundred and seventy six students provided with questionnaire, one seventy one (82%) had responded completely. The term "antimicrobial stewardship" was familiar to only 6% students. Thirty nine percent respondents correctly responded on antibacterial spectrum. Seventy two percent students mentioned that teaching on antimicrobial should begin from 3rd year and 89% felt necessity of spending more time on antimicrobials. This study revealed that future prescribers recognize the necessity of targeted teaching on antimicrobial to prepare them to prescribe antimicrobials rationally.
Introduction
The antimicrobials have been losing their effectiveness due to the emergence of resistance, which is one of the great threats to human health. This problem requires immediate intervention to delay or prevent resistance to conserve the effectiveness of available antimicrobials till development of new antimicrobial (Fishman, 2006). In Bangladesh, antimicrobials are the most widely prescribed group of medicine both at outpatient (Rahman et al., 1998) and inpatient (Afreen and Rahman, 2014). The irrationalities in route of administration and selection of expensive antimicrobials contributing additional burden on health care expenditure (Islam et al., 2007; Chowdhury et al., 2008). Antimicrobial stewardship has been advocated by scientists and organizations to improve antimicrobial prescribing to contain resistance (CDC, 2002; Carling et al., 2003; Costelloe et al., 2010; Beardsley et al., 2012; ECDPC, 2013; CDC, 2015). Infectious Disease Society of America (IDSA) defined "antimicrobial stewardship" as that optimizes the indication, selection, dosing, routes of administration and duration of antimicrobial therapy to maximize clinical cure or prevention of infection while limits the collateral damage of antimicrobial use, including toxicity , selection of pathogenic organism and emerge of resistance (Dellit et al., 2007).
Antimicrobial stewardship program helps the clinician to improve quality of care (Gordoncillo et al., 2011) and patient safety through increase rate of infection cure, reduce treatment failure and increase appropriate prescribing (Schiff et al., 2001; Hecker et al., 2003; Owens et al., 2004; Srinivasan et al., 2004; Abbo et al., 2011). The deficiency in the relevant knowledge needs to be addressed (Sharma et al., 2015) and therefore educating future prescribers about principles of antimicrobial stewardship and resistance is important (Abbo et al., 2013). These educational activities should begin during their undergraduate course with emphasis on development of critical appraisal skill to overcome the influence of pharmaceutical promotion that is considered responsible for irrational antimicrobial prescribing (Rahman, 1995; Heaton et al., 2008; O'Shaughnessy et al., 2010; Ross and Maxwell, 2012).
Due to inadequate allocation of time for antimicrobial in the undergraduate medical curriculum of Bangladesh (BMDC, 2012), the physician often learn from the practice of their colleagues and information provided by the industry (Sbarbaro, 2001). The antimicrobial stewardship should be started earlier at the time when knowledge, attitude and behavior of the prescribers are being shaped (Pulcini and Gyssens, 2013).
In Bangladesh, less importance is given on antimicrobial and emergence of resistance during teaching and evaluation both in undergraduate and postgraduate levels (Begum et al., 1999; Rahman and Huda, 2014). Though changes were suggested to improve relevance of the course content for achieving required prescribing skill of the future medical graduates, medical education system of our country has not yet adequately addressed the impending health issues (Rahman, 1995).
The aim of this study was to evaluate the knowledge and perception of future prescribers about antimicrobial stewardship and resistance, which may constitute the understanding to develop an effective intervention to educate future prescribers capable to prescribe antimicrobials in more effective and rational manner.
Materials and Methods
A cross-sectional, multicenter, questionnaire survey was conducted among 4th year medical students of Chittagong Medical College (CMC), Chattagram Maa-O-Shishu Hospital Medical College (CMOSHMC) and Southern Medical College (SMC) during January, 2016. The questionnaire was designed to evaluate the perception and knowledge regarding antimicrobial stewardship and education quality in relation to antimicrobial use and resistance in their medical colleges. The questionnaire was adopted from a previous study (Abbo et al., 2013). The questionnaire was provided to all students who attended the particular class of the studied medical colleges. Later on, the students were asked voluntarily to return the completed questionnaires in the Department of Pharmacology and Therapeutics of respective medical colleges and the anonymity of the respondents were assured.
Results
Sixty two percent of surveyed 4th year medical students (171/276) completely responded to the questionnaire. Response rates by institution were 68, 58 and 60% in CMC, CMOSHMC and SMC respectively.
Table I showed that 95% of the respondents consider that good knowledge on antimicrobial is important in their medical profession and they should have spent more time to learn about the appropriate use of antimicrobials (89%). Inappropriate use of antimicrobials (95%) and poor infection control (82%) were identified as contributors for the spread of antimicrobial resistance.
Table I: Perception of medical students about antimicrobial use and resistance
| Perceptions | All (n = 171) |
CMC (n = 68) |
CMOSHMC (n = 46) |
SMC (n = 57) |
|---|---|---|---|---|
| Resistance of antimicrobial is not an important nationwide crisis | 11 (7) |
5 (3) |
7 (3) |
9 (5) |
| Resistance of antimicrobial is not an important issue at the hospitals the respondents were placed | 42 (25) |
17 (25) |
8 (17) |
17 (29) |
| Poor infection control practices contributes to resistance of antimicrobials | 141 (82) |
56 (82) |
39 (85) |
46 (80) |
| Good quality of antimicrobial knowledge is important for professional life | 163 (95) |
65 (96) |
45 (97) |
53 (93) |
| More emphasis on the rational use of antimicrobials is needed during medical study | 152 (89) |
61 (90) |
43 (93) |
48 (85) |
| Right use of antimicrobial can also lead to resistance | 17 (12) |
7 (15) |
5 (11) |
5 (9) |
| Irrational use of antimicrobial can lead to resistance | 143 (84) |
65 (94) |
42 (93) |
48 (85) |
| Irrational use of antimicrobial causes harm to the patient | 163 (95) |
63 (92) |
44 (95) |
54 (94) |
| Prescribing of broad spectrum antimicrobials when narrow spectrum antimicrobials are effective leads to resistance | 161 (94) |
66 (97) |
44 (95) |
51 (90) |
| Problems of antimicrobial resistance can be reduced if antimicrobials are prescribed rationally | 155 (91) |
65 (96) |
42 (90) |
48 (85) |
| Percentage of respondents who have the same opinion with mentioned statement | ||||
About 72% of the participants opined in favor of beginning the teaching on antimicrobial from the third year of medical course. More than half (59%) of the students claim themselves well-prepared to identify and use reliable sources of information on treatment of infections and the basic mechanisms of antimicrobial resistance (60%). Almost all (95%) respondents recalled that formal lectures on antimicrobial and their rational use was taken. Only 12% respondents know time to start antimicrobials, 9% about how to select the right duration and 15% about how to select the correct doses of antimicrobials. Only 56% participants can select correct spectrum for different antimicrobials and felt well-prepared to streamline and de-escalate antimicrobial therapy (Table II).
Table II: Perception and knowledge of medical students' regarding educational activities required for preparedness of antimicrobial stewardship
| Perception and knowledge | All (n = 171) |
CMC (n = 68) |
CMOSHMC (n = 46) |
SMC (n = 57) |
|---|---|---|---|---|
| Know about the reliable sources of information | 101 (59) |
41 (60) |
23 (50) |
37 (65) |
| Have attended formal lectures on antimicrobial use | 162 (95) |
65 (96) |
45 (97) |
52 (92) |
| Have attended lecture on how to select right dose and duration of antimicrobial | 16 (9) |
4 (4) |
4 (10) |
8 (15) |
| Can select appropriate antimicrobial for a selective infection | 51 (30) |
17 (25) |
14 (30) |
20 (35) |
| Know appropriate time to initiate antibiotic treatment | 20 (12) |
8 (12) |
5 (10) |
7 (13) |
| Can differentiate antimicrobial spectrum | 95 (56) |
41 (60) |
23 (50) |
31 (55) |
| Able to switch of intravenous to oral therapy | 31 (18) |
14 (20) |
7 (15) |
10 (18) |
| Can streamline antimicrobial treatment | 95 (53) |
24 (36) |
12 (25) |
17 (30) |
| Can interpret culture sensitivity report | 110 (64) |
45 (66) |
30 (65) |
35 (62) |
| Able to manage patient demanding unnecessary antimicrobials | 23 (13) |
11 (15) |
5 (10) |
7 (12) |
| Opined that teaching about antimicrobial should start from 3rd year | 123 (72) |
47 (69) |
32 (70) |
44 (77) |
| Proportion of participants who sense that their medical is good enough | ||||
The most commonly used resources were text book (65, 60 and 68%) and smart phone applications (48, 35 and 25%) among students of CMC, CMOSHMC and SMC respectively. Forty one percent used Wikipedia (40, 45 and 38%) in CMC, CMOSHMC and SMC respectively. Familiarity with the Antimicrobial Guideline of Bangabandhu Sheikh Mujib Medical University was 18, 15 and 20% among students of CMC, CMOSHMC and SMC respectively (Table III).
Table III: Resources used to learn about antimicrobial prescribing and resistance
| Resources | All (n = 171) |
CMC (n = 68) |
CMOSHMC (n = 46) |
SMC (n = 57) |
|---|---|---|---|---|
| Medical journals | 35 (20) |
14 (20) |
12 (25) |
9 (15) |
| Senior students | 61 (36) |
27 (40) |
14 (30) |
20 (35) |
| Antimicrobial guidelines of BSMMU | 31 (18) |
12 (18) |
7 (15) |
12 (20) |
| Guidelines of other institutions | 36 (21) |
14 (20) |
9 (20) |
13 (22) |
| Textbooks | 111 (65) |
44 (65) |
28 (60) |
39 (68) |
| Wikipedia | 70 (41) |
27 (40) |
21 (45) |
22 (38) |
| Pharmaceutical representatives | 21 (12) |
7 (10) |
5) (10) |
9 (15) |
| Smart phone application | 52 (37) |
32 (48) |
16 (35) |
14 (25) |
| Percentage of respondents who often or sometimes used the mentioned resource | ||||
About risks associated with antimicrobial use, diagnosis and treatment of community-acquired pneumonia 32% responded rightly, which are 26% in case of urinary tract infections. Thirty nine percent were correct about spectrum of activity of commonly used antimicrobials. Eighty eight percent respondents can distinguish the possible risks associated with unnecessary use of antimicrobials (Table IV).
Table IV: Knowledge relevant to clinical decision reflected by the proportion of correct response about the selection of antimicrobials
| Knowledge about antimicrobials and ability of clinical decision | All (n = 171) |
CMC (n = 68) |
CMOSHMC (n = 46) |
SMC (n = 57) |
|---|---|---|---|---|
| Able to categorize problems associated with inappropriate use of antimicrobials | 130 (76) |
49 (72) |
35 (75) |
46 (80) |
| Able to identify spectrum of antimicrobials | 67 (39) |
24 (36) |
20 (42) |
23 (40) |
| Able to recognize risk associated with irrational use of antimicrobials | 150 (88) |
60 (88) |
42 (90) |
48 (85) |
| Able to select appropriate antimicrobial in community acquired pneumonia and know about switching from intravenous to oral therapy | 55 (32) |
22 (32) |
16 (36) |
17 (30) |
| Able to select appropriate antimicrobial in complicated UTI and know about duration of therapy | 45 (26) |
22 (32) |
12 (26) |
11 (20) |
| Able to select appropriate antimicrobial against β- lactamase producing E. coli becteremia | 49 (29) |
17 (25) |
14 (30) |
18 (32) |
| Percentage of respondents who were capable to respond correctly to the questions related to clinical knowledge | ||||
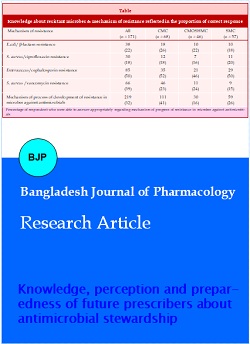
On questions regarding mechanisms of antimicrobial resistance, 22, 18, 50 and 39% respondents replied correctly on questions about resistance of E. coli against beta-lactam antimicrobials, S. aureus against ciprofloxacin, Enterococcus against cephalosporin and S. aureus against vancomycin respectively (Table V).
Table V: Knowledge about resistant microbes & mechanism of resistance reflected in the proportion of correct response
| Mechanism of resistance | All (n = 171) |
CMC (n = 68) |
CMOSHMC (n = 46) |
SMC (n = 57) |
|---|---|---|---|---|
| E.coli/ beta-lactam resistance | 38 (22) |
18 (26) |
10 (22) |
10 (18) |
| S. aureus/ciprofloxacin resistance | 30 (18) |
12 (18) |
7 (16) |
11 (20) |
| Enterococcus/cephalosporin resistance | 85 (50) |
35 (52) |
21 (46) |
29 (50) |
| S. aureus /vancomycin resistance | 66 (39) |
46 (23) |
11 (24) |
9 (15) |
| Mechanism of process of development of resistance in microbes against antimicrobials | 219 (32) |
111 (41) |
30 (16) |
59 (26) |
| Percentage of respondent who were able to answer appropriately regarding mechanism of progress of resistance in microbes against antimicrobials | ||||
Discussion
The present study revealed that medical students of different medical colleges share similar perceptions toward antimicrobial stewardship and resistance across medical colleges. A previous study conducted among 5th year medical students demonstrated that their knowledge was satisfactory (71.3, 67.2 and 57.9%) on clinical use of antimicrobials, "theory on resistance" and "antimicrobial spectrum" (Rahman and Huda, 2014). The present study revealed that the term "antimicrobial stewardship" was familiar to only six percents of participant which indicate absence of the issue in the curriculum as well as lack of awareness among the teachers about the most widely accepted approach of resistance containment (Rahman, 1995; CDC, 2002; Rahman and Huda, 2014). Most of the participants mentioned that knowledge about antimicrobial (95%) and its’ rational use (90%) is important in their medical profession, which reflect the concern and awareness of future prescribers about the magnitude and importance of the issue.
Inappropriate use of antimicrobials (95%) was mentioned as cause of emergence of antimicrobial resistance, which was shown in a survey conducted in the USA. That study also revealed that the magnitude of appropriate utilization of antimicrobial was recognized by the student (Abbo et al., 2013). One study conducted among British medical students showed that they urge for more education targeted on antimicrobial prescribing, which was reflected in the revised curriculum where efforts were made to increase student awareness (Heaton et al., 2008).
Only few students know about time to initiate antibiotic therapy, length of antibiotic therapy and the appropriate doses, which reveal that the exiting teaching could not contributed satisfactorily on these crucial issues. The students opined that teaching about antimicrobial should begin at their early student life like 3rd or 4th year of MBBS course.
Prescribers of Bangladesh usually diagnose microbial infection on clinical judgment and select antimicrobial empirically which unfavorably affect the sensitivity pattern of microbes (Faiz and Rahman, 2004). To prevent the antimicrobial resistance, in addition to doctors, the knowledge and perception of other health professionals also need to be updated (Wester et al., 2002; Srinivasan et al., 2004; Pulcini et al., 2011). There are many aspects of infection management, which require multidisciplinary approach. Pharmacologist, microbiologist, epidemiologist and molecular biologist should work together while designing strategies to prevent antimicrobial resistance (Rahman and Huda, 2014). Pharmacologists especially should start incorporating the regulatory issues in academic discussion to make the teaching more relevant to the real life situation of the future prescribers (Rahman, 1995).
This study reflected the opinions of the 4th year medical students who have completed their antimicrobial related portion of academic curriculum, i.e., Pharmacology and Therapeutics and Microbiology. Thus, this study provided a better approximation of their current medical education, though potential recall bias on self report could not be overcome and the reason of non-response was not explored.
Medical students have a positive perception and awareness about the consequence of antibiotic resistance and also conscious about their potential role in antimicrobial resistance containing activities. In order to overcome these identified deficiencies, the undergraduate medical curriculum needs to address these issues at appropriate step or level of medical course. According to these observations, the undergraduate medical curriculum may consider incorporating and emphasizing teaching-learning program on principles of antimicrobial stewardship and resistance to improve prescribing.
Conclusion
Particular emphasis should be given on time to start, proper selection, duration and rational use of antimicrobials, which program should be started earlier when medical student's knowledge and attitude are being formed. The present study might help to develop a framework for inclusion of "antimicrobial stewardship" into medical curriculum.
References
Abbo L, Sinkowitz-Cochran R, Smith L, Ariza-Heredia E, Gomez-Marin O, Srinivasan A, Hooton TM. Faculty and resident physicians' attitudes, perceptions, and knowledge about antimicrobial use and resistance. Infect Control Hosp Epidemiol. 2011; 32: 714-18.
Abbo LM, Cosgrove SE, Pottinger PS, Pereyra M, Sinkowitz-cochran R, Srinivasan A, Webb DJ, Hooton TM. Medical students' perceptions and knowledge about antimicrobial stewardship: How are we educating our future prescribers? Clin Infect Dis. 2013; 57: 631-38.
Afreen S, Rahman MS. Patterns of medicine use in patients of common respiratory diseases treated in the Department of Pediatrics of BSMMU hospital. Bangladesh J Physiol Pharmacol. 2014: 30: 9-13.
Bangladesh Medical & Dental Council (BMDC). Curriculum for undergraduate medical education in Bangladesh-updated 2012, approved and published in September 2012, pp 140-67.
Beardsley JR, Williamson JC, Johnson JW, Luther VP, wren RH, Ohl CC. Show me the money: Long-term financial impact of an antimicrobial stewardship program. Infect Control Hosp Epidemiol. 2012; 33: 398-400.
Begum M, Rahman MS, Islam AFMS, Khan IA, Akhter N. Eleven years of the undergraduate medical curriculum. 1988: Review on the changes in pharmacology written questions. Bangladesh J Physiol Pharmacol. 1999; 15: 27-30.
Carling P, Fung T, Killion A, Terrin N, Barza M. Favorable impact of a multidisciplinary antibiotic management program conducted during 7 years. Infect Control Hosp Epidemiol. 2003; 24: 699-706.
Center for Disease Control and Prevention (CDC). CDC's campaign to prevent antimicrobial resistance in health care settings. MMWR Morb Mortal Wkly Rep. 2002; 51: 343.
Center for Disease Control and Prevention (CDC). Get smart: Know when antibiotics work. Available at: http://www.cdc.gov/getsmart/antibiotic-use/index.html. Accessed 18 March 2015.
Chowdhury AK, Rahman MS, Faroque AB, Hasan GA, Raihan SZ. Excessive use of avoidable therapeutic injections in the Upazilla health complexes of Bangladesh. Mymensingh Med J. 2008: 17(Suppl 2): S59-64.
Costelloe C, Metcalfe C, Lovering A, Mant D, Hay AD. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patient: Systemic review and meta-analysis. Br Med J. 2010; 340: c2096.
Dellit TH, Owens RC, McGowan JE Jr, Gerding DN, Weinstein RA, Burke JP, Huskins WC, Paterson DL, Fishman NO, Carpenter CF, Brennan PJ, Billeter M, Hooton TM. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007; 44: 159-77.
European Centre for Disease Prevention and Control (ECDPC). European Antibiotic Awareness Day. Available at: http://ecdc.europa.eu/en/EAAD/Pages/Home.aspx. 2013 Accessed on 4th February, 2016.
Faiz MA, Rahman MR. Rational antimicrobial use. J CMCTA. 2004; 15: 1-3.
Fishman N. Antimicrobial Stewardship. Am J infect Cont. 2006; 34: SS55-63.
Gordoncillo MJ, Bender J, Noffsinger J, Bartlett PC. Developing an open-access antimicrobial resistance learning site for veterinary medical students. J Vet Med Educ. 2011; 38: 404-07.
Heaton A, Webb DJ, Maxwell SR. Undergraduate preparation for prescribing: The views of 2413 UK medical students and recent graduates. Br J Clin Pharmacol. 2008; 66: 128-34.
Hecker MT, Aron DC, Patel NP, Lehmann MK, Donskey CJ. Unnecessary use of antimicrobials in hospitalized patients: Current patterns of misuse with an emphasis on the antianaerobic spectrum of activity. Arch Intern Med. 2003; 163: 972-78.
Islam MS, Rahman MS, Misbahuddin M. Impact of prescription audit & feedback on pattern of prophylactic antimicrobials in caesarean section: A cost reduction perspective. Bangladesh J Physiol Pharmacol. 2007; 23: 1-9.
O'Shaughnessy L, Haq I, Maxwell S, Llewelyn M. Teaching of clinical pharmacology and therapeutics in UK medical schools: Current status in 2009. Br J Clin Pharmacol. 2010; 70: 143-48.
Owens RC Jr, Fraser GL, Stogsdill P. Antimicrobial stewardship program as a means to optimize antimicrobial use. Insights from the society of infectious diseases pharmacists. Pharmacotherapy 2004; 24: 896-908.
Pulcini C, Gyssens IC. How to educate prescribers in antimicrobial stewardship practices, Virulence. 2013; 4: 192-202.
Pulcini C, Williams F, Molinari N, Davey P, Nathwani D. Junior doctors' knowledge and perceptions of antibiotic resistance and prescribing: A survey in France and Scotland. Clin Microbiol Infect. 2011; 17: 80-87.
Rahman MS, Begum M, Khan IA, Chowdhury S, Islam AMZ, Sultana R, Hoque MZ, Akhter N. A baseline survey on the use of drugs at private practitioner level in Bangladesh. Bangladesh J Physiol Pharmacol. 1998: 14: 47-50.
Rahman MS, Huda S. Antimicrobial resistance and related issues: An overview of Bangladesh situation. Bangladesh J Pharmacol. 2014; 9: 218-24.
Rahman MS. Changes required in pharmacotherapy teaching to ensure rational use of drugs. Bangladesh J Physiol Pharmacol. 1995; 11: 38-39.
Ross S, Maxwell S. Prescribing and the core curriculum for tomorrow's doctors: BPS curriculum in clinical pharmacology and prescribing for medical students. Br J Clin Pharmacol. 2012; 74: 644-61.
Sbarbaro JA. Can we influence prescribing patterns? Clin Infect Dis. 2001; 33: 240-44.
Schiff GD, Wisniewski M, Bult J, Parada JP, Aggarwal H, Schwartz DN. Improving inpatient antibiotic prescribing: Insights from participation in a national collaborative. Jt Comm J Qual Improv. 2001; 27: 387-402.
Sharma K, Jain P, Sharma A. Knowledge, attitude and perception of medical and dental undergraduates about antimicrobial stewardship. Ind J Pharmacol. 2015; 47: 676-79.
Srinivasan A, Song X, Richard A, Sinkowitz-Cochran R, Cardo D, Rand C. A survey of knowledge, attitudes, and beliefs of house staff physicians from various specialties concerning antimicrobial use and resistance. Arch Intern Med. 2004; 164: 1451-56.
Wester CW, Durairaj L, Evans AT, Schwartz DN, Husain S, Martinez E. Antibiotic resistance: A survey of physician perceptions. Arch Intern Med. 2002; 162: 2210-16.