Berberine hydrochloride inhibits inflammatory response via regulating the miRNA-140-5p/TLR4/NF-κB signaling pathway in oral lichen planus
Abstract
The present study investigates the anti-inflammatory mechanism of berberine hydrochloride in the oral lichen planus. The local inflammatory environment of the oral lichen planus was mimicked, through which lipopolysaccharides stimulated keratinocyte HaCaT cells. Berberine hydrochloride suppressed the activation of the TLR4/NF-κB inflammatory signaling pathway by up-regulating miRNA-140-5p, which is an independent risk factor for the oral lichen planus. Furthermore, miRNA-140-5p inhibited the TLR4/NF-κB inflammatory signaling pathway by directly suppressing TLR4 expression. Therefore, the present study suggests that berberine hydrochloride inhibits the inflammatory response by up-regulating miRNA-140-5p to suppress the activation of the TLR4/NF-κB inflammatory signaling pathway in the oral lichen planus.
Introduction
The oral lichen planus is a disease of the oral mucosa caused by the chronic inflammatory response mediated by immune cells (Mignogna et al., 2004; Liu et al. 2010; Wang et al., 2016). It is well-known that nuclear factor-kappa β (NF-κβ) and NF-κB-related cytokines, such as tumor necrosis factor–α (TNF-α), interleukin (IL)-6 and IL-8, play an important role in regulating the inflammation in the pathological process (Chang et al., 2016; Hay et al., 2016; Shen et al., 2016). The activation of the NF-κB signaling pathway is positively correlated with the activation and recruitment of cytotoxic T lymphocytes. Toll-like receptor (TLR) activation is a major factor for the activation of the NF-κB signaling pathway (Wang et al., 2016). After stimulation by different TLR ligands, NF-κB is released into the nucleus of cells, which in turn activates a variety of inflammatory mediators, such as pro-inflammatory factors and chemokines (Cao et al., 2017; Du et al., 2017). Among these inflammatory mediators, TNF-α, a main cytokine, can regulate the paracrine and autocrine of inflammatory mediators, such as IL-1, IL-6 and IL-8, which induce cell damage as a cytotoxic substance (Charrad et al., 2016; Robert et al., 2016). Therefore, it can be considered that the TLR4/NF-κB signaling pathway plays an important role in the progression of oral lichen planus, and that this can be used as a target to inhibit the expression of inflammatory mediators in the course of oral lichen planus, in order to alleviate local tissue damage.
Oral lichen planus remains uncured. In recent years, the significant effect of plant extracts on anti-immunotherapy has received increasing attention by scholars. Berberine hydrochloride extracted from Coptis chinensis has been widely used in the treatment of various autoimmune diseases (Ren et al., 2011, Li et al., 2014). Recent studies have shown that berberine hydrochloride can inhibit the production of proinflammatory cytokines to inhibit acute and chronic inflammation, including delayed allergic reaction and experimental autoimmune tubulointerstitial nephritis, suggesting that berberine hydrochloride has an immuno-suppressive effect (Li et al., 2014). Some researchers have revealed that berberine hydrochloride not only inhibits the proliferation and activation of lymphocytes, but also inhibits the production of cytokines, such as INF-γ, TNF-α and IL-2. Therefore, berberine hydrochloride may inhibit the inflammatory response through the TLR4/ NF-κB signaling pathway, thereby alleviating the symptoms of oral lichen planus (Qin et al., 2015; Choi, 2016). However, the regulation mechanism by which berberine hydrochloride regulates the TLR4/NF-κB signaling pathway remains unclear.
MicroRNA (miRNA) is well-known for its involvement in regulating the expression of target genes, either by degrading a specific mRNA, or inhibiting mRNA translation (Zhang et al. 2016). A number of studies have revealed that abnormal miRNA expression is closely correlated to multiple diseases, such as cancer, diabetes and systemic lupus erythematosus (Li et al., 2017). However, miRNA can affect inflammation by regulating signaling pathways (Kurozumi et al., 2016). Hesperidin alleviates lipopolysaccharide (LPS)-induced neuroinflammation in mice by promoting the miRNA-132 signaling pathway (Li et al., 2016). Therefore, the investigators hypothesized that the regulation of the TLR4/NF-κB signaling pathway by berberine hydrochloride may be mediated by the miRNA.
In the present study, an oral lichen planus model stimulated by LPS was done to explore a) the anti-inflammatory effect of berberine hydrochloride on oral lichen planus, and b) the associated molecular mechanisms of berberine hydrochloride in its anti-inflammatory effect.
Materials and Methods
Patients and clinical samples
The study was conducted on 130 healthy subjects and 130 oral lichen planus patients from January 2015 to September 2017. The clinicopathological characteristics of patients and healthy subjects are presented in Table I. Oral mucosa tissues with a size of 5 × 5 mm were collected from oral lichen planus patients under local anesthesia, while normal oral mucosa tissues were collected from healthy subjects under local anesthesia. All tissue samples were immediately frozen in liquid nitrogen, and stored at -80°C until using.
Table I: Clinicopathological characteristics
| Clinical variable | Oral lichen planus (n=130) |
Healthy subjects (n=130) |
|---|---|---|
| Age (year) | 52.7±15.4 | 51.4±16.2 |
| Gender | ||
| Male | 41 | 45 |
| Female | 89 | 85 |
| Course of disease (month) | 6-36 | - |
| Smoke | 53 | 59 |
| Drink | 78 | 73 |
| Position | ||
| Single site | 59 | - |
| Cheek | 49 | - |
| Tongue | 7 | - |
| Floor of mouth | 2 | - |
| Lip | 1 | - |
| Multiple sites | 71 | - |
| Clinical classification | ||
| Single form | 95 | - |
| Erosive type | 46 | - |
| Reticular striation | 27 | - |
| Atrophic type | 9 | - |
| Patch type | 9 | - |
| Papular type | 4 | - |
| Multi form | 35 | - |
Cell line and culture
The HaCaT cell line was provided by the American Type Culture Collection (ATCC, USA). HaCaT cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM; Gibco, USA) with 10% fetal bovine serum (FBS; Gibco, USA) at 37°C in a humidified atmosphere with 5% CO2. In order to simulate the local immune microenvironment of oral lichen planus, the culture medium was replaced with keratinocyte serum-free medium (KSFM; Gibco, USA), in which HaCaT cells were cultured overnight, and stimulated with lipopolysaccharide (LPS; Aladdin, China) at a concentration of 10 μg/mL for 48 hours. Then, the HaCaT cells were treated with berberine hydrochloride (0, 5, 10 and 20 mg/L) for two hours. Afterwards, these cells were harvested for the subsequent experiments.
RNA isolation and RT–qPCR
According to the manufacturer’s instructions in the RNA Extraction Kit (Lexogen, China), the total RNA was extracted from HaCaT cells and oral mucosa tissues. Then, the complementary DNA was transcribed and amplified with the specific sense and antisense general primer. The cycling conditions included the following: 95°C for 3 min, 45 cycles of 95°C for 15 sec, and 58°C for 15 sec (miRNA-140-5p) or 60°C for 15 sec (IL-6, TNF-α and TLR4), and subsequently, 72°C for 10 sec. The mRNA level, when compared to controls, was calculated using the following equation: fold expression level = 2 – ΔΔCt. The polymerase chain reaction (PCR) reactions for each gene were repeated in triplicate, and independent experiments were performed for three times.
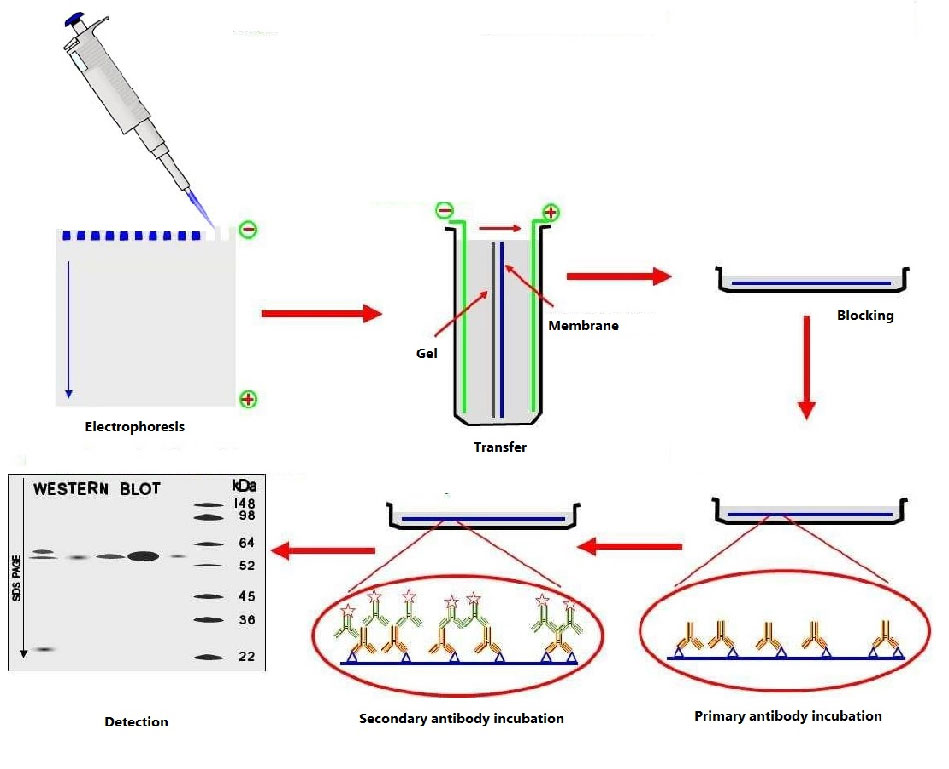
Box 1: Western Blotting Analysis
PrincipleWestern blotting analysis uses the electrophoretic transfer of proteins from sodium dodecyl sulfate polyacrylamide gels to sheets of polyvinylidene fluoride or nitrocellullose membrane, followed by immunodetection of proteins using antibodies with fluorescent or chemiluminescent detection.
Requirements
Anti-MYD88 antibody (Abcam, USA); Anti-p-IκB antibody (Huabio, China); Anti-p-P56 antibody (Santa Cruz, USA); Anti-TLR4 antibody (Abcam, USA); Anti-β-actin antibody (Huabio, China); BCA protein assay kit (Transgen, China); FITC anti-mouse (Invitrogen, USA); HaCaT cells; iBright Imaging Systems (Thermo Fisher, USA); Polyvinylidene fluoride membrane (Bio-Rad, USA); SDS-PAGE (Thermo Fisher Scientific, USA);
Procedure
Protein extraction
Step 1: HaCaT cells (number of cells) collected from the 10 cm petri dish.
Step 2: Add 1 mL of protein lysate containing protease inhibitor, shake gently, and lyse on ice for 15-30 min.
Step 3: Scrape adherent cells off the dish using a cold plastic cell scraper, then gently transfer the cell suspension into a 1.5 mL Eppendorf tube, then place the tube on ice. Any bubble within it should be avoided.
Step 4: The collected cells can also be fully lysed by sonication with 10% power (650 W), over 2 sec, stop for 3 sec. Place the ultrasound probe in the middle of the sample lysate, but do not touch the tube wall or tube bottom for ultrasound. The intracellular suspension of 1 mL should be sonicated for 10-25 cycles.
Step 5: Centrifuge at 12,000 rpm for 10-15 min at 4℃.
Step 6: Gently aspirate the supernatant to another fresh tube and place on ice for later use. Be careful not to absorb impurities such as lipids floating in the upper layer.
Protein quantification using BCA protein assay kit
Step 1: Prepare the BCA working reagent by mixing BCA reagent A with reagent B in a ratio of 50:1 (V/V), and incubate for 24 hours at room temperature.
Step 2: Dissolve the standard to a final concentration of 0.5 mg/L with the same solvent used for samples.
Step 3: Pipette gradient volume of standard solution (0, 1, 2, 4, 8, 12, 16 and 20 μL) to microplate wells, and add standard diluent to each well to final volume 20 μL.
Step 4: Pipette 200 μL BCA working reagent to each well and incubate at 37℃ for 30 min.
Step 5: Measure absorbance at 562 nm using spectrophoto-meter.
Step 6: Calculate protein concentration based on the standard curve.
Separation of protein
Step 1: Then, 50 μg of total protein were separated by 10% SDS-PAGE.
Transfer of protein from the gel to membrane
Step 3: After transferring onto the polyvinylidene fluoride membrane, blocking was performed with 5% skim milk. Detection of antigen loaded blotting membrane
Step 4: The primary antibodies (anti-TLR4 antibody, anti-p-P56 antibody, anti-MYD88 antibody, anti-p-IκB antibody, anti-β-actin antibody) were incubated overnight at 4°C.
Analysis of antigen-antibody specific binding
Step 5: The secondary antibodies conjugated with FITC were added and fixed for 60 min.
Step 6: The signal was detected using iBright Imaging Systems.
References (video)
Cao and Zheng, 2016; Cui et al., 2016
Stable expression of miRNA-140-5p
Lentiviral vectors, which overexpress miRNA-140-5p, were purchased from Hanbio (China). The lentiviral vector expressing scrambled RNA was purchased as a control. HaCaT cells were infected with the lentiviral vector. Then, fluorescence-activated cell sorting flow cytometry was used to select polyclonal cells with green fluorescent protein signals. The miRNA-140-5p levels from these cell clones was quantified using RT–qPCR.
Luciferase reporter assay
The TLR4 3’-UTR fragment (1,601 bp) amplified by the PCR primers (sense: 5′-TCTGGGGAGGCACATCTTCT-3′, antisense: 5′-AGGTCCAAGTTGCCGTTTCT-3′) was cloned into psiCHECK-2 vectors (WT). The GeneTailor Site-Directed Mutagenesis System (Invitrogen, USA) was used to perform the site-directed mutagenesis of miRNA-140-5p (site in TLR4 3′-UTR; MT). For the reporter assay, the MT or WT vector and control vector, psiCHECK-2 vector, were transfected into K562 cells with the miRNA-140-5p mimics or miRNA-140-5p inhibitors in 48-well plates. At two days after the transfection, K562 cells were harvested for the luciferase assay. The Dual-Luciferase Reporter Assay System (Active Motif, USA) was used for the luciferase assay, according to manufacturer’s protocol.
Statistical analysis
All assays were independently performed in triplicate. IBM SPSS 21.0 software and Origin 9.0 were used for all statistical analyses. Student’s t-test and X2-test were used for the significant differences between groups. The multivariate logistic model was used to evaluate the independent risk factor. Two-sided p values were calculated, and a probability level of 0.05 was set for the statistical significance.
Results
Effect on the TLR4/NF-κB inflammatory signaling pathway
The results in Figure 1A show that the mRNA level of IL-6 and TNF-α significantly increased in HaCaT cells after LPS stimulation (Figure 1A). Meanwhile, the protein expression level of p-P65, TLR4 and p-IκB significantly increased (Figure 1B). More importantly, it was found that the level of IL-6, TNF-α, p-P65, TLR4 and p-IκB significantly increased in oral lichen planus keratinocytes relative to the keratinocytes received from healthy mucosal tissues (Figures 1C and D). These results show that the oral lichen planus inflammatory model was established with the activation of the TLR4/NF-κB inflammatory signaling pathway.
Figure 1: The relative expression level of inflammatory cytokines. (A) The mRNA expression level of IL-6 and TNF-α in oral lichen planus inflammatory model stimulated by LPS. (B) The protein expression level of p-P65, TLR4 and p-IκB in oral lichen planus inflammatory model stimulated by LPS. (C) The mRNA expression level of IL-6 and TNF-α in oral lichen planus patients and healthy subjects. (D) The protein expression level of p-P65, TLR4 and p-IκB in oral lichen planus patients and healthy subjects
The mRNA level of IL-6 and TNF-α significantly decreased in a dose-related fashion with the increase in berberine hydrochloride concentration, suggesting that berberine hydrochloride could reduce the production of inflammatory cytokines (Figures 2A and B).
The protein expression of p-P65, TLR4 and p-IκB was significantly down-regulated with the treatment of berberine hydrochloride (Figure 2C). These results suggest that berberine hydrochloride can suppress the activation of the TLR4/NF-κB inflammatory signaling pathway.
Figure 2: The relative expression level of inflammatory cytokines after treating with berberine hydrochloride. (A) The mRNA expression level of IL-6 after treating with different concentration of berberine hydrochloride. (B) The mRNA expression level of TNF-α after treating with different concentration of berberine hydrochloride. (C) The mRNA expression level of p-P65, TLR4 and p-IκB after treating with berberine hydrochloride (20 mg/L). (D) The level of miRNA-140-5p after treating with different concentration of berberine hydrochloride
Effects on the level of miRNA-140-5p
In order to delineate the regulation mechanism by which berberine hydrochloride suppresses the TLR4/NF-κB inflammatory signaling pathway, the miRNA level of regulating proteins in the TLR4/NF-κB inflammatory signaling pathway between the oral lichen planus inflammatory model and oral lichen planus inflammatory model treated with berberine hydrochloride was investigated. MiRNAs were searched using the bioinformatics tool, TargetScanHuman (http:// http://www.targetscan.org)(Table II): 12 miRNAs were predicted to regulate P65, while there was a significant difference of five miRNAs between the two groups; three miRNAs were predicted to regulate MYD88, while there was a significant difference of one miRNA between the two groups; nine miRNAs were predicted to regulate IκB, while there was a significant difference of four miRNAs between the two groups; one miRNA was predicted to regulate TLR4, while there was a significant difference of this miRNA between the two groups. Furthermore, the level of miR-140-5p presented with the largest difference. It was further revealed that the level of miRNA-140-5p significantly increased in a dose-related fashion with the increase in berberine hydrochloride concentration (Figure 2D). These results suggest that berberine hydrochloride inhibits the TLR4/NF-κB inflammatory signaling pathway via up-regulating miRNA-140-5p in the oral lichen planus.
Table II: Expression difference of miRNAs in oral lichen planus inflammatory model before and after treatment
| Protein | miRNA | Before treatment | After treatment | p value |
|---|---|---|---|---|
| P65 | miRNA-520a-3p | 1.0 ± 0.3 | 2.0 ± 0.5 | <0.05 |
| miRNA-520d-3p | 1.3 ± 0.2 | 1.4 ± 0.2 | >0.05 | |
| miRNA-520e | 1.2 ± 0.3 | 1.4 ± 0.3 | >0.05 | |
| miRNA-520c-3p | 1.3 ± 0.2 | 1.4 ± 0.4 | >0.05 | |
| miRNA-520b | 0.5 ± 0.1 | 0.3 ± 0.1 | >0.05 | |
| miRNA-302e | 0.6 ± 0.1 | 1.1 ± 0.2 | <0.05 | |
| miRNA-302b-3p | 1.2 ± 0.3 | 0.6 ± 0.1 | <0.05 | |
| miRNA-302d-3p | 1.2 ± 0.1 | 1.1 ± 0.2 | >0.05 | |
| miRNA-372-3p | 1.1 ± 0.1 | 1.0 ± 0.3 | >0.05 | |
| miRNA-373-3p | 1.2 ± 0.5 | 2.5 ± 0.1 | <0.05 | |
| miRNA-302a-3p | 1.2 ± 0.2 | 2.7 ± 0.4 | <0.05 | |
| miRNA-302c-3p.1 | 0.9 ± 0.2 | 1.0 ± 0.3 | >0.05 | |
| TLR4 | miRNA-140-5p | 1.5 ± 0.2 | 4.3 ± 0.4 | <0.05 |
| MYD88 | miRNA-6504-5p | 1.0 ± 0.2 | 1.7 ± 0.2 | <0.05 |
| miRNA-3064-5p | 1.2 ± 0.2 | 1.4 ± 0.2 | >0.05 | |
| miRNA-182-5p | 0.6 ± 0.1 | 0.8 ± 0.1 | >0.05 | |
| IκB | miRNA-300 | 1.7 ± 0.3 | 1.5 ± 0.3 | >0.05 |
| miRNA-381-3p | 1.8 ± 0.1 | 1.1 ± 0.3 | <0.05 | |
| miRNA-493-5p | 1.7 ± 0.2 | 1.4 ± 0.3 | >0.05 | |
| miRNA-532-3p | 1.6 ± 0.3 | 1.4 ± 0.2 | >0.05 | |
| miRNA-378d | 1.4 ± 0.2 | 1.4 ± 0.2 | >0.05 | |
| miRNA-378c | 1.0 ± 0.3 | 1.7 ± 0.2 | <0.05 | |
| miRNA-378i | 2.0 ± 0.4 | 2.2 ± 0.3 | >0.05 | |
| miRNA-378f | 2.2 ± 0.2 | 0.9 ± 0.3 | <0.05 | |
| miRNA-378b | 1.4 ± 0.3 | 2.1 ± 0.2 | >0.05 |
Relationship between the development of oral lichen planus and miRNA-140-5p
The development of oral lichen planus was significantly correlated with the psychological factor, gastritis, physical and chemical stimulation, autonomic nerve disorder and miRNA-140-5p level (p<0.05)(Table III). However, there was no significant association between oral lichen planus development and oral hygiene, hepatitis, diabetes and cardiovascular disease (p>0.05).
Table III: Analysis of risk factors for oral lichen planus
| Clinical variable | Oral lichen planus (n=130) |
Healthy volunteer (n=130) |
p value |
|---|---|---|---|
| Psychological factor | 47 | 11 | p<0.05 |
| Oral hygiene | 12 | 9 | NS |
| Gastritis | 55 | 13 | p<0.05 |
| Hepatitis | 6 | 5 | NS |
| Diabetes | 8 | 9 | NS |
| Angiocardiopathy | 11 | 12 | NS |
| Physical and chemical stimulation | 81 | 34 | p<0.05 |
| Autonomic nerve | 36 | 11 | p<0.05 |
| miRNA-140-5p | 1.43 ± 0.46 | 3.28 ± 0.82 | p<0.05 |
| NS: Not significant | |||
The multivariate logistic model analysis revealed that psychological factor, gastritis, physical and chemical stimulation, autonomic nerve disorder and miRNA-140-5p were risk factors for oral lichen planus (Table IV). Taken together, these observations thereby suggest that the down-regulation of miRNA-140-5p is responsible for oral lichen planus development.
Table IV: Logistic regression analysis of related risk factors in oral lichen planus patients
| Clinical variable | HR | 95% CI | P value |
|---|---|---|---|
| Psychological factor | 0.148 | 0.071-0.398 | p<0.05 |
| Gastritis | 0.213 | 0.113-0.572 | |
| Physical and chemical stimulation | 0.165 | 0.093-0.482 | |
| Autonomic nerve disorder | 0.138 | 0.066-0.438 | |
| miRNA-140-5p | 0.087 | 0.005-0.316 |
Effect of MiRNA-140-5p on NF-κBp65 expression by binding to its 3’UTR
In order to delineate the underlying molecular mechanism by which the up-regulation of miRNA-140-5p was responsible for inhibiting the inflammatory signaling pathway, the target of miRNA-140-5p was further verified. A dual-luciferase reporter system was used to confirm whether miRNA-140-5p mediated the expression of TLR4. The 3’-UTR region of the TLR4 mRNA, including the MUT site or the WT site, was co-transfected with the miRNA-140-5p mimics (Figure 3A). The luciferase reporter system (Figure 3B) revealed that the reporter plasmid with the TLR4 WT site resulted in a definite decrease in luciferase activity with the transfection of miRNA-140-5p mimics. However, few changes in luciferase activity was observed after the co-transfection of the TLR4 MUT site and miRNA-140-5p mimics. Subsequently, the mRNA and protein expression levels of TLR4 were measured by up-regulating miRNA-140-5p or silencing miRNA-140-5p. The TLR4 mRNA and protein levels significantly decreased with the up-regulation of miRNA-140-5p (Figures 3C and D). In contrast, the down-regulation of miRNA-140-5p level resulted in the increase in miRNA-140-5p mRNA and protein level. The data from this part of the present study thereby demonstrate that miRNA-140-5p can directly suppress TLR4 expression by binding to its 3’UTR. In order to confirm the inhibition effect of miRNA-140-5p on the TLR4/NF-κB inflammatory signaling pathway, the proteins expression level of the TLR4/NF-κB inflammatory signaling pathway with the up-regulation of miRNA-140-5p was measured. The expression level of MyD88, p-IκB, p-P65, IL-6 and TNF-α significantly increased in the oral lichen planus inflammatory model with the up-regulation of miRNA-140-5p (Figures 4A and 4B). These results indicate that miRNA-140-5p could inhibit the TLR4/NF-κB inflammatory signaling pathway by directly suppressing the TLR4 expression.
Figure 3: miRNA-140-5p inhibits inflammatory reaction in oral lichen planus via directly inhibiting expression of TLR4. (A) Sequence alignment between miRNA-140-5p and the 3′-UTR of TLR4 mRNA. (B) The effect of miRNA-140-5p on the activity of luciferase reporter containing either WT or MUT 3′-UTR was examined by luciferase reporter gene assays. The effect of miRNA-140-5p on the endogenous expression levels of TLR4 was examined in oral lichen planus inflammatory model by RT–qPCR (C) and Western blot (D)
Figure 4: Ectopic expression of miRNA-140-5p inhibition of inflammatory reaction. (A) Overexpression of miRNA-140-5p increased the mRNA level of IL-6 and TNF-α in oral lichen planus inflammatory model. (B) Western blot showing that changes of miRNA-140-5p expression influenced the expression of MYD88, p-IκB and p-P65
Discussion
Clinical observation has revealed that oral lichen planus with long-term erosion and ulcer recurrence can be significantly alleviated after infusion of anti-inflammatory, indicating that inflammation aggravates the symptoms of oral lichen planus, but is not conducive to disease control (Gupta et al., 2017; He et al., 2017). Significantly, several studies have shown that berberine hydrochloride can inhibit acute and chronic inflammation, enhance nonspecific immune response, and inhibit cellular immunity and humoral immunity in mice (Liang et al., 2016; Wang et al., 2018). For example, Cao et al. reported that berberine hydrochloride could attenuate lipopolysaccharide-induced endometritis in mice by suppressing the activation of the NF-κB signaling pathway (Fu et al., 2015). However, the treatment effect and anti-inflammatory mechanism of berberine hydrochloride in oral lichen planus has not been determined.
Berberine hydrochloride significantly decreased the level of IL-6 and TNF-α, and suppressed the activation of the TLR4/NF-κB inflammatory signaling pathway. Furthermore, the miRNA-140-5p that targeted to NF-κBp65 was distinguished using the bioinformatics tool TargetScanHuman. More importantly, miRNA-140-5p could serve as an independent risk factor for oral lichen planus, and the level of miRNA-140-5p was significantly increased after the treatment of berberine hydrochloride in the oral lichen planus inflammatory model. In addition, it was confirmed that miRNA-140-5p could directly suppress NF-κBp65 expression by binding to its 3’UTR, and the up-regulation of miRNA-140-5p inhibited the TLR4/NF-κB inflammatory signaling pathway. Therefore, berberine hydrochloride inhibits inflammatory response by upregulating miRNA-140-5p to suppress the activation of the TLR4/NF-κB inflammatory signaling pathway in oral lichen planus.
The clinical symptom of oral lichen planus is inflammation disease, which chronically, persistently and recurrently attacks. It has been reported that CD8+ cytotoxic T lymphocyte directly attacks basal keratinocytes, which result in the liquefaction and degeneration of keratinocytes. The release of cytokines, such as interferonγ, TNF-α, colony-stimulating factor and IL-6, promotes local inflammation and aggravates tissue damage (Zhou et al., 2016; Polesello et al., 2017). Therefore, an oral lichen planus inflammatory model was established to evaluate the treatment effect and anti-inflammatory mechanism of berberine hydrochloride. LPS, a potential cell activator, can activate multiple target cells in tissues, which is beneficial for the secretion of various inflammatory cytokines that trigger local inflammatory responses (Hwang et al., 2016, Marchini et al., 2016). Hence, LPS was used to stimulate keratinocytes HaCaT cells. The present study revealed that the lichen planus inflammatory model had a significantly high expression of TNF-α and IL-6, while the TLR4/NF-κB inflammatory signaling pathway was found to be activated, which was in accordance to previous studies. In the present study, it was found that berberine hydrochloride significantly decreased the level of TNF-α and IL-6. More importantly, it was found that the activation of the TLR4/NF-κB inflammatory signaling pathway was inhibited. These present results are consistent with previous studies. For example, Yu et al. reported that berberine hydrochloride induces anti-inflammatory effects by inhibiting the TLR4/NF-κB inflammatory signaling pathway in an LPS-induced murine model of mastitis (Wang et al., 2018). However, the mechanism by which berberine hydrochloride regulates the factors in the TLR4/NF-κB inflammatory signaling pathway remains unclear.
MiRNA, a small non-coding RNA molecule, participates in post transcriptional gene expression regulation via base-pairing with complementary sequences within mRNA molecules (Bockhorn et al., 2017). Wang et al. reported that miRNA-129-5p inhibits the development of autoimmune encephalomyelitis-related epilepsy by targeting HMGB1 through the TLR4/NF-kB signaling pathway (Liu et al., 2017). Meanwhile, Gao et al. reported that the anti-Inflammatory activity of tanshinone IIA is induced via miRNAs and the TLR4/NF-κB signaling pathway in LPS-stimulated RAW264.7 macrophages (Fan et al., 2016). Therefore, it was hypothesized that the inhibition effect of berberine hydrochloride on the TLR4/NF-κB signaling pathway is via miRNAs in the oral lichen planus. In order to prove this hypothesis, the miRNAs that target factors of the TLR4/NF-κB inflammatory signaling pathway were determined using bioinformatics tool TargetScanHuman. It was found that the level of miRNA-140-5p was significantly increased in the oral lichen planus inflammatory model with the treatment of berberine hydrochloride. Previous studies have shown that miRNA-140-5p inhibits synovial fibroblast proliferation and inflammatory cytokine secretion by targeting TLR4 (Li et al., 2017). In order to further prove the hypothesis, the correlation between the expression of miRNA-140-5p and the development of oral lichen planus was assessed. The present analysis results revealed that miRNA-140-5p is an independent risk factor for oral lichen planus. Subsequently, the mechanisms by which miRNA-140-5p regulated the expression of TLR4 were further investigated. It was found that the ectopic expression of miRNA-140-5p reduced the level of TLR4 and inhibited the TLR4/NF-κB inflammatory signaling pathway. However, the regulation mechanism by which berberine hydrochloride upregulates the level of miRNA-140-5p remains unclear. Various studies have shown that berberine hydrochloride can bind to nucleic acids (He et al., 2017). Hence, it was hypothesized that berberine hydrochloride may inhibit miRNA-140-5p degradation, which increases the level of miRNA-140-5p. The regulatory mechanism by which berberine hydrochloride up-regulates the level of miRNA-140-5p still needs further studies in the future.
Conclusion
Mimic inflammatory responses through which LPS stimulates HaCaT cells were established, and it was found that berberine hydrochloride exhibits a potential therapeutic effect on the oral lichen planus by reducing the secretion of inflammatory cytokines and inhibiting the activation of the TLR4/NF-κB inflammatory signaling pathway. Furthermore, it was identified that a miRNA, miRNA-140-5p, was up-regulated by berberine hydrochloride, and this is an independent risk factor for oral lichen planus. miRNA-140-5p could inhibit the TLR4/NF-κB inflammatory signaling pathway by directly suppressing NF-κBp65 expression in oral lichen planus.
Ethical Issue
The ethics approval for the present study was approved by the Departmental discussion on 13 March 2015 (Reference No. 2015031301), and all oral lichen planus patients and healthy subjects provided a written informed consent.
References
Bockhorn J, Dalton R, Nwachukwu C, Huang S, Prat A, Yee K, Chang YF, Huo D, Wen Y, Swanson KE. MicroRNA-30c inhibits human breast tumour chemotherapy resistance by regulating TWF1 and IL-11. Nat Commun. 2017; 4: 1393.
Cao T, Zhang H, Zhou L, Wang Y, Du G, Yao H, Wang Y, Luo Q, Chen F, Wang W. In vitro cell culture system optimization of keratinocytes from oral lichen planus (OLP) patients. Oral Dis. 2017; 23: 225-32.
Cao XD, Zheng HM. Zerumbone inhibits prostate cancer cell viability and induces cell death by non-apoptotic pathway. Bangladesh J Pharmacol. 2016; 11: 771-75.
Chang JY, Chen IC, Wang YP, Wu YH, Chen HM, Sun A. Anemia and hematinic deficiencies in gastric parietal cell antibody-positive and antibody-negative erosive oral lichen planus patients with thyroid antibody positivity. J Formos Med Assoc. 2016; 115: 1004-11.
Charrad R, Berraïes A, Hamdi B, Ammar J, Hamzaoui K, Hamzaoui A. Anti-inflammatory activity of IL-37 in asthmatic children: Correlation with inflammatory cytokines TNF-α, IL-β, IL-6 and IL-17A. Immunobiology 2016; 221: 182-87.
Choi YH. Berberine hydrochloride protects C2C12 myoblast cells against oxidative stress-induced damage via induction of Nrf-2-mediated HO-1 expression. Drug Dev Res. 2016; 77: 310-18.
Cui Y, Ren H, Li HC, Wang QS. Artemisinic acid exhibits antitumor activity in MCF-7 breast cancer cells through the inhibition of angiogenesis, VEGF, m-TOR and AKT signaling pathways. Bangladesh J Pharmacol. 2016; 11: 691-96.
Du J, Li R, Yu F, Yang F, Wang J, Chen Q, Wang X, Zhao B, Zhang F. Experimental study on 1,25(OH)2 D3 amelioration of oral lichen planus through regulating NF-κB signaling pathway. Oral Dis. 2017; 23: 770-78.
Fan G, Jiang X, Wu X, Fordjour PA, Miao L, Zhang H, Zhu Y, Gao X. Anti-inflammatory activity of tanshinone IIA in LPS-stimulated RAW264.7 macrophages via miRNAs and TLR4-NF-κB pathway. Inflammation. 2016; 39: 375-84.
Fu K, Lv X, Li W, Wang Y, Li H, Tian W, Cao R. Berberine hydrochloride attenuates lipopolysaccharide-induced endometritis in mice by suppressing activation of NF-κB signal pathway. Int Immunopharmacol. 2015; 24: 128-32.
Gupta S, Ghosh S, Gupta S. Interventions for the management of oral lichen planus: A review of the conventional and novel therapies. Oral Dis. 2017; 23: 1029-42.
Hay RA, Rashed L, Hegazy R, Rashwan W, Samir N, Nour-Edin F. Association of interleukin (IL)18 and IL10 gene polymorphisms with oral lichen planus risk: A case-control study. J Dermatol Sci. 2016; 83: 244-47.
He Y, Gong D, Shi C, Shao F, Shi J, Fei J. Dysbiosis of oral buccal mucosa microbiota in patients with oral lichen planus. Oral Dis. 2017; 23: 674-82.
Hwang JH, Kim KJ, Ryu SJ, Lee BY. Caffeine prevents LPS-induced inflammatory responses in RAW264.7 cells and zebrafish. Chem Biol Interact. 2016; 248: 1-7.
Kurozumi A, Goto Y, Matsushita R, Fukumoto I, Kato M, Nishikawa R, Sakamoto S, Enokida H, Nakagawa M, Ichikawa T. Tumor-suppressive microRNA-223 inhibits cancer cell migration and invasion by targeting ITGA3/ITGB1 signaling in prostate cancer. Cancer Sci. 2016; 107: 84-94.
Li H, Guan SB, Lu Y, Wang F. MiR-140-5p inhibits synovial fibroblasts proliferation and inflammatory cytokines secretion through targeting TLR4. Biomed Pharmacother. 2017; 96: 208-14.
Li M, Shao H, Zhang X, Qin B. Hesperidin alleviates lipopolysaccharide-induced neuroinflammation in mice by promoting the miRNA-132 pathway. Inflammation. 2016; 39: 1-9.
Li X, Zhao SJ, Shi HL, Qiu SP, Xie JQ, Wu H, Zhang BB, Wang ZT, Yuan JY, Wu XJ. Berberine hydrochloride IL-8 dependently inhibits invasion and IL-8-independently promotes cell apoptosis in MDA-MB-231 cells. Oncol Rep. 2014; 32: 2777-88.
Li Y, Chen Y, Li J, Zhang Z, Huang C, Lian G, Yang K, Chen S, Lin Y, Wang L. Co-delivery of microRNA-21 antisense oligonucleotides and gemcitabine using nanomedicine for pancreatic cancer therapy. Cancer Sci. 2017; 108: 1493-503.
Liang S, Kuang Y, Ma F, Chen S, Long Y. A sensitive spectrofluorometric method for detection of berberine hydrochloride using Ag nanoclusters directed by natural fish sperm DNA. Biosens Bioelectron. 2016; 85: 758-63.
Liu AH, Wu YT, Wang YP. MicroRNA-129-5p inhibits the development of autoimmune encephalomyelitis-related epilepsy by targeting HMGB1 through the TLR4/NF-kB signaling pathway. Brain Res Bull. 2017; 132: 139-49.
Liu Y, Messadi DV, Wu H, Hu S. Oral lichen planus is a unique disease model for studying chronic inflammation and oral cancer. Med Hypotheses. 2010; 75: 492-94.
Marchini C, Angeletti M, Eleuteri AM, Fedeli A, Fioretti E. Aspirin modulates LPS-induced nitric oxide release in rat glial cells. Neurosci Lett. 2016; 381: 86-91.
Mignogna MD, Fedele S, Lo Russo L, Lo Muzio L, Bucci E. Immune activation and chronic inflammation as the cause of malignancy in oral lichen planus: Is there any evidence? Oral Oncol. 2004; 40: 120-30.
Polesello V, Zupin L, Di LR, Biasotto M, Pozzato G, Ottaviani G, Gobbo M, Crovella S, Segat L. DEFB1 polymorphisms and salivary hBD-1 concentration in oral lichen planus patients and healthy subjects. Arch Oral Biol. 2017; 73: 161-65.
Qin W, Song Y, Dai Y, Qiu G, Ren M, Zeng P. Treatment of berberine hydrochloride pharmaceutical wastewater by O3 /UV/H2O2 advanced oxidation process. Environ Earth Sci. 2015; 73: 4939-46.
Ren M, Song Y, Xiao S, Ping Z, Peng J. Treatment of berberine hydrochloride wastewater by using pulse electrocoagulation process with Fe electrode. Chem Eng J. 2011; 169: 84-90.
Robert S, Gicquel T, Bodin A, Lagente V, Boichot E. Characterization of the MMP/TIMP imbalance and collagen production induced by IL-1β or TNF-α release from human hepatic stellate cells. PloS One. 2016; 2016.
Shen Z, Du G, Zhou Z, Liu W, Shi L, Xu H. Aberrant expression of interleukin-22 and its targeting microRNAs in oral lichen planus: A preliminary study. J Oral Pathol Med. 2016; 45: 523-27.
Wang H, Zhang D, Han Q, Zhao X, Zeng X, Xu Y, Sun Z, Chen Q. Role of distinct CD4+ T helper subset in pathogenesis of oral lichen planus. J Oral Pathol Med. 2016; 45: 385-93.
Wang X, Feng S, Ding N, He Y, Li C, Li M, Ding X, Ding H, Li J, Wu J. Anti-Inflammatory effects of berberine hydrochloride in an LPS-induced murine model of mastitis. Evid Based Complement Alternat Med. 2018; 2018: 5164314.
Wang Y, Wen B, Yu H, Ding D, Zhang J, Zhang Y, Zhao L, Zhang W. Berberine hydrochloride-loaded chitosan nano-particles effectively targets and suppresses human nasopharyngeal carcinoma. J Biomed Nanotechnol. 2018; 14: 1486-95.
Wang Y, Zhang H, Du G, Wang Y, Cao T, Luo Q, Chen J, Chen F, Tang G. Total glucosides of paeony (TGP) inhibits the production of inflammatory cytokines in oral lichen planus by suppressing the NF-κB signaling pathway. Int Immunopharmacol. 2016; 36: 67-72.
Zhang J, Jima DD, Jacobs C, Fischer R, Gottwein E, Huang G, Lugar PL, Lagoo AS, Rizzieri DA, Friedman DR. Patterns of microRNA expression characterize stages of human B-cell differentiation. Blood. 2016; 113: 4586-94.
Zhou L, Cao T, Wang Y, Yao H, Du G, Chen G, Niu X, Tang G. Frequently increased but functionally impaired CD4+ CD25+ regulatory T cells in patients with oral lichen planus. Inflammation 2016; 39: 1205-15.