Systematic review and meta-analysis of shenqi fuzheng and chemotherapy combination in the treatment of breast cancer
Abstract
This review evaluates the effectiveness and safety of injection of shenqi fuzheng with chemotherapy in the treatment of breast cancer in China. The study included 20 randomized clinical trials (RCTs) involving 1,609 patients. It was shown that shenqi fuzheng could improved the treatment efficiency, Kamofsky Performance Status (KPS), weight and autoimmune; reduced fatigue, gastrointestinal reaction and the toxicity of bone marrow; protected liver, kidney and heart from damage by chemotherapy. However, the quality of all the studies was relatively low and there was great heterogeneity between various studies. Further well-designed research is needed to estimate the beneficial effects of shenqi fuzheng.
Introduction
The morbidity of breast cancer had been more than cervical cancer in many Western countries and had been highest in gynecological tumors (Pu et al., 2015). Cancer statistics show that breast cancer is the most frequently diagnosed cancers (Horton et al., 2015). A total of 565,469 cancer deaths were reported in USA in 2008, for which practical data are effective at the most recent years (Lee et al., 2014). Cancer is the second leading cause of death (23% of all death) following heart disease. From 2007 to 2008, the cancer death rate reduced 1.5%, from 178.4/100,000 to 175.8 (Raia-Barjat et al., 2014). At present, the incidence of breast cancer rose by 3-4% each year which was higher than the global average growth rate in China (Valadares et al., 2013).
Chemotherapy has been an important method of adjuvant treatment of breast cancer. It has a lot of problems in the use to treat breast cancer (Schmidt et al., 2015). Toxic and adverse effects of chemotherapy have a strong impact on adjuvant treatment of breast cancer. Some patients cannot accomplish treatment in accordance with the original plans of adjuvant treatment of breast cancer (von Minckwitz et al., 2014). When chemotherapeutics acted on the tissues of breast cancer patient, its specific inhibitory effects on cancer cell were weaker. At the same time, chemotherapeutics could kill a large number of normal cells of breast cancer, so with the result that sufferers usually complain nausea, vomiting, inappetence, leukopenia, multiple organ function lesion, and exhaustion syndrome (McCarthy et al., 2014).
Reduce the adverse effects of chemotherapy is important in the treatment of breast cancer. Shenqi fuzheng mainly contains pilose asiabell root and Mongolian milkvetch root. It has cardioprotection, antifatigue, immunity enhancement, replenishing blood, increase the function of spleen and kidney, improve the secretion of hematopoietic factor and lymphocyte, extend survival of cell and so on (Yao et al., 2014). Pharmacological studies have shown that pilose asiabell root and Mongolian milkvetch root can activate T-cell and enhance macrophage phagocytosis, improve the body's immune function, adjust the metabolism of body cell, have fight oxidation and inhibit the bone marrow toxicity of chemotherapy drugs and so on (Ai et al., 2014). Astragalus inhibits the proliferation of breast cancer cell lines (MDA-MB-468; MDA-MB-231). At the same time, the effects of astragalus on MDA-MB-468 cell and mMSCs are related to the concentration of astragalus (Deng and Chen, 2009) and its mechanism of inhibiting the proliferation of MDA-MB-468 cell might be due to down-regulation of the expressions of EGFR and p53 protein (Ye and Chen, 2008).
At present, the quality of many RCT with shenqi fuzheng and chemotherapy combination in the treatment of breast cancer was uneven. At the same time, there was system assessment about shenqi fuzheng combined with chemotherapy in the treatment of breast cancer. Therefore, it is necessary to make a system evaluation of RCT of shenqi fuzheng combined with chemotherapy in the treatment of breast cancer, and provide a reference for clinic treatment and future studies.
Materials and Methods
Literature search
The following databases were used for literature search: CBM, CNKI, VIP, Wangfang Data, Springer Link, EBSCO, PubMed, MEDLINE and Embase. The selected RCT of shenqi fuzheng combined with chemotherapy in the treatment of breast cancer were collected. The reference lists of papers were authenticated and scanned for further trials. The under search labels were used conjunctively or individually: "Postoperative breast cancer", "Breast Cancer", "Chemotherapy", "Shenqi fuzheng injection", "Randomized controlled trial", and "Clinical trial". All of these literatures were updated up to May, 2015.
Inclusion criteria: All the articles of RCT about shenqi fuzheng in the treatment of breast cancer with chemotherapy were assessed including the following parameters: the object of study: the female breast cancer patients; the intervening measure of experimental group: shenqi fuzheng plus standard chemotherapy; the intervening measure of control group: the standard chemotherapy; the assessment criteria: the treatment efficiency, physical condition autoimmunity, protected main organs, reduced the toxicity of bone marrow, etc; the course of treatment >4 weeks; full-text document.
Exclusion criteria: The literatures that had been not included were as follows: the duplicate publication literature; the literature could not provide the basic information of subjects or the relevant information of intervening measure.
Quality assessment
Two authors independently worked for literature searching, studied choice, and extraction of data. When there was any disagreement, then it was solved by discussion. Xing Li guided the overall process of this study. The abstracted data included were as follows: title, authors, time of publication, information on methodology, sex, control interventions, treatment, outcomes and adverse drug reaction. The assessment tool was used to assess all studies to address the following seven criteria (Cochrane 5.1.0 Handbook of Systematic Reviews of Interventions): randomization, allocation concealment, blinding, loss of imitation and exit cases, intention-to-treat analysis, baseline and Cochrane score. These studies which met the standards were a) low risk of bias, b) unclear risk of bias, c) high risk of bias, and if insufficient information acquired to make judgment.
Data extraction
We read the title, summary as well as full text of all included studies to extract the data. Two researchers independently conducted the quality assessment and discussed the quality of each paper with each other and finally made a decision.
Data analysis
RevMan 5.2 software was used for meta-analysis. Clinical heterogeneity and methodological heterogeneity of the included studies were analyzed. When statistical results with p value <0.05, the difference was considered as statistically significant. Meta-analysis was utilized if the studies had receivable homogeneity of study design, controls, interventions, participants, and outcome measures. The heterogeneity test results, p<0.1, I2 >50%, we adopted random effects model (REM); p>0.1, I2 <50%, we adopted fixed effect model (FEM) (Shui et al., 2015). Data was summarized using risk ratio (RR) with 95% confidence intervals (CI) for binary outcomes or mean difference (MD) with a 95% CI for continuous outcomes. Publication bias was explored by way of a funnel-plot analysis (Pu et al., 2014). Missing or lost to cases count data should be counted as treatment failure cases. So, we have demonstrated the sensitivity analysis, if the research indicators contained more than 10 RCT and used funnel plot to check the presence of publication bias; if research indicators contained less than 10 RCT and did not check.
Results
Studies
Seven databases were searched for screening of 1,497 documents. Duplicate documents (1,019) were eliminated by way of hand searches and electronic. The eliminated 959 documents were "time too long" or the "no-research object". We eliminated non-randomized controlled trial/interventions and the results have not met the inclusion criteria by reading abstract (60 documents). We eliminated 27 documents with data in question/random method is not correct by reading full text. Finally full-text papers of 20 studies were searched from all the citations. A flow chart described the search method and study chose (Figure 1).
Figure 1: Flowchart of identification of studies included in the review
General characteristics
There were 20 trials literature containing 1,609 cases (shenqi fuzheng group: 831 cases and chemotherapy group: 778 cases). In this study, the largest number of cases in RCT was 185 and the least number was 40. The features of studies were mentioned in Table I.
Table I: Baseline characteristics of the eligible trials
| Reference | Randomization | Allocation concealment | Form of double-blind | Loss of imitation and exit cases | ITT analysis | Baseline | Cochrane score |
|---|---|---|---|---|---|---|---|
| Xiao et al., 2005 | Mention | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Chen et al., 2007 | Mention | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Xu et al., 2010 | Mention | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Chen et al., 2010 | Mention | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Yuan et al., 2008 | Random number | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Lie et al., 2005 | Mention | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Kawuli et al., 2011 | Mention | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Zhu et al., 2007 | Random number | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Xu et al., 2003 | Mention | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Lu et al., 2010 | Mention | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Zhang et al., 2004 | Mention | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Wang et al., 2006 | Random number | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Zou et al., 2006 | Mention | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Li et al., 2004 | Mention | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Sun et al., 2011 | Mention | Unclear | Unclear | Clear | Unclear | Yes | C |
| Li et al., 2002 | Random number | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Cui et al., 2011 | Mention | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Ze et al., 2011 | Mention | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Huang et al., 2008 | Random number | Unclear | Unclear | Unclear | Unclear | Yes | C |
| Dai et al., 2007 | Mention | Unclear | Unclear | Unclear | Unclear | Yes | C |
Quality of methodology of RCT
We made a system evaluation of all the included studies in accordance with the "Cochrane 5.1.0 Handbook of Systematic Reviews". All the included studies were categorized to low risk of bias. All studies had no sample estimate and belonged to low quality (Table II).
Table II: Methodological quality scores
| Reference | Sample size (Rx = C) | Age (Year, Rx = C) | Experimental intervention | Control intervention | Duration of treatments |
|---|---|---|---|---|---|
| Xiao et al., 2005 | 55/53 | 56.7 | SI + CEF | CEF | 8 days SI; 8 days CEF |
| Chen et al., 2007 | 34/34 | 51 | SI + CEF | CEF | 6 x 24 days SI; 6 x 21 days CEF |
| Xu et al., 2010 | 28/24 | 47/49 | SI + TA | TA | 7 days SI; 21 days TA |
| Chen et al., 2010 | 90/95 | 42/45 | SI + TD | TD | 2~3 days SI; 21 days TD |
| Yuan et al., 2008 | 38/35 | 38/35 | SI + CAF | CAF | 3 x 20 days SI; 3 x 20 days CAF |
| Lie et al., 2005 | 30/30 | 56/57 | SI + 5-FU + Navelbine | 5-FU + Navelbine | 7 days SI; m 21 day 5-FU + Navelbine |
| Kawuli et al., 2011 | 40/40 | 46 | SI + TA | TA | 3 x 7 days SI; 3 x 21 days TA |
| Zhu et al., 2007 | 32/24 | 52.5/51 | SI + CEF | CEF | 4 x 10 days SI; 4 x 21 days CEF |
| Xu et al., 2003 | 53/59 | - | SI + CAF | CAF | 8 days SI; 21 days CAF |
| Lu et al., 2010 | 58/52 | 58.5 | SI + CAF | CAF | 2~3 x 2 weeks SI; 2~3 x 3 weeks CAF |
| Zhang et al., 2004 | 26/30 | - | SI + CAF | CAF | 8 days SI; 21 days CAF |
| Wang et al., 2006 | 40/32 | 45.2 ± 9.8/46.7 + 10.5 | SI + CMF | CMF | 6 x 8 days SI; 6 x 21 days CMF |
| Zou et al., 2006 | 32/32 | 52.5 | SI + CTE | CTE | 2 x 14 days SI; 2 x 14 days CTE |
| Li et al., 2004 | 40/35 | 56.4/54.2 | SI + NE | NE | 10 days SI; 3 x 28 days NE |
| Sun et al., 2011 | 60/45 | 55 | SI + CMF | CMF | 4 x 28 days SI; 4 x 28 days CMF |
| Li et al., 2002 | 35/27 | 47.2 ± 10.8/46.7 ± 10.5 | SI + CAF | SI + CAF | 3 x 21 days SI; 3 x 21 days CAF |
| Cui et al., 2011 | 22/20 | 52 | SI + CAF, AC | FAC, AC | 4 x 5 ~8 days SI; 4 x 21 days FAC, AC |
| Ze et al., 2011 | 23/20 | 43 | SI + Chemotherapy | Chemotherapy | 2-4 x 10 days SI;2-4 x 21 days Chemotherapy |
| Huang et al., 2008 | 30/30 | 47/46 | SI + CTF | CTF | 2 x 28 days SI; 2 x 28 days CTF |
| Dai et al., 2007 | 65/61 | 45.5 ± 26.8/46.1 ± 27.5 | SI + CEF | SI + CEF | 2 x 28 days SI; 2 x 28 days CEF |
Meta-analysis
Effective treatment: Five trials (526 patients) reported the effectiveness of shenqi fuzheng treatment (180/265) and shenqi fuzheng combined with chemotherapy (138/261). The heterogeneity test results p=0.04, I2=60%, we had chosen fixed effect model (FEM). Z=2.35, RR =1.35, 95%CI [1.05~1.73], p=0.02. The results showed, the treatment efficiency of shenqi fuzheng combined with chemotherapy in treatment of breast cancer was significantly higher than the control group, compared the difference was significant (Figure 2).
Figure 2: Treatment efficiency of SI in treatment of breast cancer with chemotherapy
Nutritional status
Kamofsky performance status: The eight trials reported that shenqi fuzheng improved patient's Kamofsky performance status in treatment of breast cancer with chemotherapy, which included 610 patients, shenqi fuzheng group and chemotherapy group were 253/321, 143/289, respectively. The heterogeneity test results p=0.42, I2=1%, we had chosen FEM. Z=7.00, RR=1.58, 95% CI [1.39~1.79], p<0.00001. The results show, shenqi fuzheng was significantly higher than the control group in treatment of breast cancer patient's Kamofsky Performance Status with chemotherapy, compared the difference was significant (Figure 3).
Figure 3: KPS of SI in treatment of breast cancer with chemotherapy
Weight gain: The two trials reported that shenqi fuzheng gained patient's weight in the treatment of breast cancer with chemotherapy, which included 218 patients, shenqi fuzheng group and chemotherapy group were 93/113, 32/105, respectively. The heterogeneity test results p=0.10, I2=63%, we had chosen REM. Z=3.79, RR=2.70, 95% CI [1.62~4.52], p<0.00001. The results show, that shenqi fuzheng was significantly higher than the control group in treatment of breast cancer patient's weight with chemotherapy, compared the difference were significant (Figure 4).
Figure 4: The weight of SI in treatment of breast cancer with chemotherapy
Reduction of fatigue: The two trials reported that shenqi fuzheng reduced patient's fatigue in treatment of breast cancer with chemotherapy, which included 132 patients, shenqi fuzheng group and chemotherapy group were 23/66, 52/66, respectively. The heterogeneity test results p=0.12, I2=58%, we had chosen REM. Z=2.71, RR=0.44, 95% CI [0.24~0.79], p=0.007. The results show, shenqi fuzheng was significantly higher than the control group in treatment of breast cancer patient's fatigue with chemotherapy, compared the difference was significant (Figure 5).
Figure 5: The fatigue of SI in treatment of breast cancer with chemotherapy
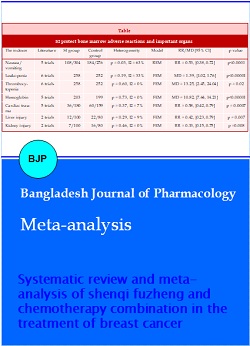
Protect the bone marrow suppression situation and the important organs of the patient: Shenqi fuzheng could protect effectively breast cancer patient's bone marrow adverse reactions and important organs during chemotherapy, was significantly higher than the control group, compared the difference was significant. These adverse reactions included nausea and vomiting, leukopenia, thrombocytopenia, decreased hemoglobin, cardiac injury, liver injury and kidney injury (Table III).
Table III: SI protect bone marrow adverse reactions and important organs
| The indexes | Literature | SI group | Control group | Heterogeneity | Model | RR/MD [95% CI] | p value |
|---|---|---|---|---|---|---|---|
| Nausea/vomiting | 5 trials | 108/304 | 184/276 | p = 0.03, I2 = 63% | REM | RR = 0.53, [0.38, 0.72] | p<0.0001 |
| Leukopenia | 6 trials | 258 | 252 | p = 0.19, I2 = 33% | FEM | MD = 1.39, [1.02, 1.76] | p<0.00001 |
| Thrombocytopenia | 6 trials | 258 | 252 | p = 0.60, I2 = 0% | FEM | MD = 13.25, [2.45, 24.04] | p = 0.02 |
| Hemoglobin | 5 trials | 203 | 199 | p = 0.73, I2 = 0% | FEM | MD = 10.82, [7.44, 14.21] | p<0.00001 |
| Cardiac trauma | 5 trials | 36/180 | 60/159 | p = 0.37, I2 = 7% | FEM | RR = 0.58, [0.42, 0.79] | p = 0.0007 |
| Liver injury | 2 trials | 12/100 | 22/80 | p = 0.29, I2 = 9% | FEM | RR = 0.42, [0.23, 0.79] | p = 0.007 |
| Kidney injury | 2 trials | 7/100 | 16/80 | p = 0.46, I2 = 0% | FEM | RR = 0.33, [0.15, 0.75] | p =0.008 |
Activity of T cell subsets and NK cells: In summary, shenqi fuzheng could increase effectively the activity of breast cancer patient's T cell and NK cells during chemotherapy, was significantly higher than the control group, compared the difference was significant (Table IV).
Table IV: SI increase the activity of breast cancer patient's T cell and NK cells
| Time | Number of trials | SI group/Control group | Heterogeneity | Model | MD [95% CI] | p value |
|---|---|---|---|---|---|---|
| CD3 | 5 | 263/256 | p = 0.03, I2 = 61% | REM | 9.60 [8.66, 10.53] | p<0.00001 |
| CD4 | 6 | 205/185 | p<0.00001, I2 = 94% | REM | 11.43 [10.51, 12.35] | p<0.0001 |
| CD8 | 4 | 182/168 | p<0.00001, I2 = 96% | REM | 4.29 [3.50, 5.07] | p<0.00001 |
| CD4/CD8 | 7 | 310/298 | p = 0.26, I2 = 23% | FEM | 11.43 [10.51, 12.35] | p<0.00001 |
| NK cells | 5 | 228/214 | p<0.00001, I2 = 84% | REM | 6.01 [3.26, 8.76] | p<0.0001 |
Heterogeneity analysis: The study had 16 indicators in which 7 indicators (I2 <25%) were considered good homogeneity and developed a meta-analysis. 1 indicator (25%<I2<50%) was considered mild heterogeneity and chosen FEM. 5 indicators (50%<I2<75%) were considered moderate heterogeneity and chosen REM. 3 indicators (I2>75%) was considered high heterogeneity and chosen REM. We analyzed the causes of heterogeneity and found that methods, technological means and time of measurement were very variable in different years and different areas. These differences might bring about heterogeneity of these indicators in the study. At the same time, the evaluation criterions of better homogeneity indicators was relatively objective, so their study result had good homogeneity.
Discussion
Chemotherapeutics have cytotoxicity, can inhibit tumor cell growth and kill normal cells, and restrain hematopoietic system (Sanchez et al., 2014). At the same time, chemotherapeutics can treat breast cancer with traditional Chinese medical science, which can reduce significantly side effects and ensure the completion of chemotherapy treatment (Li et al., 2015).
Shenqi fuzheng can promote proliferation role of T cell subsets and improve the T cell immunity. Shenqi fuzheng often used to cure various kinds of immunocompromised patients in clinical, such as recurrent respiratory tract infection, postoperation of chemotherapy and radiotherapy, and chronic and serious illness. Shenqi fuzheng can improve the body's immune function, shorten the course and invigorate health effectively of breast cancer (Bo et al., 2007). Many researches show that Mongolian milkvetch root can produce erythrocyte and granulocyte of bone marrow cells, treat significantly leucopenia (Xie et al., 2011). Pilose asiabell root can increase the red blood cells, white blood cells and hemoglobin. Shenqi fuzheng has supporting the healthy energy, “Yiqi Jianpiâ€, antifatigue, adjustion of humoral and cell-mediated immunity, protection of bone marrow function, and reduces adverse effects of chemotherapeutics to heart by means of angiectasis and improve circulation (Lin et al., 2013). Modern pharmacology explain that Mongolian milkvetch root can improve directly or indirectly the ability of adrenal cortex and has a strengthening and restoring and promoting the health effect. Mongolian milkvetch root can improve the antineoplastic activity by means of increased proliferation of T cell and increase the capability of lymphocyte transformation (Lu and Chen, 2003).
Comprehensive literature evaluation, clinical effects of shenqi fuzheng combined with chemotherapy in treatment of breast cancer included: shenqi fuzheng could enhance treatment efficiency (p=0.02); shenqi fuzheng could improve the nutritional situation of patient, improve patient's Kamofsky performance status (p<0.00001) and weight (p=0.0002), and reduce patient's fatigue (p=0.007); shenqi fuzheng could protect the bone marrow suppression situation of patient, increase the number of leucocyte (p<0.00001), hematoblast (p=0.02) and hemoglobin (p<0.00001), and reduce nausea and vomiting (p<0.0001); shenqi fuzheng could protect the main organs, protect the liver (p=0.007), kidney (p=0.008) and heart (p=0.0007); shenqi fuzheng could increase the activity of T cell subsets and NK cells (p<0.00001).
The evidence-based medicine emphasizes that scientific evidence should be organically combined with clinician's decision-making and patients' own intents. The conclusion of this study pays more attention to the statistical significance and differences. Before clinical application, experts and scholars' experience of diagnosis and treatment should be combined, and patients' own intents should also be fully considered to comprehensively evaluate the clinical significance of this conclusion.
In the 20 RCT included in this evaluation, 4 studies (5/20) described the specific random method, the other experiments mention "Random". None reported allocation concealment, double-blind method, ITT analysis, and loss of imitation and exit cases. Baseline of all studies was no difference. However, the intention-to-treat principle was not adopted for data analysis. All the included RCT have the word "random" in their reports, but they neither describe the randomized order nor the allocation concealment. And only part of them mentions about the used random methods. While in the RCT published in domestic core journals, coverage rate of the randomized order is 48.9% (Schulz, 2001). Improper use of random method or false random may cause selective bias and have enormous influences upon the test results. Randomized allocation concealment in foreign RCT is as high as 48%. Allocation concealment also plays an important role in preventing bias and randomization. Without allocation concealment, the intervention effect can be exaggerated by an average of 30-41% (Moher et al., 2010). This is the deficiency of the study. At the same time, all documents are compared with the patients' baseline data, such as the pathological grading and staging and treatment plan, the results have shown that the baselines between experimental group and the control group are comparable (p>0.05).
These 20 trials literature included the average number of 41.6 cases in shenqi fuzheng plus chemotherapy group and 38.9 cases in chemotherapy group. 5 studies (5/20%) were study population >100 cases. There were no the estimated sample size in all research. Sample size of all trials was too small, which increased incidence of type II error and reduced the accuracy of the test results. This is the inadequate research. At same time, the important factor was the low-quality RCT.
In the 20 RCT included in this systematic review, only 14 RCT took the pathological diagnosis as the standard for the judgment of breast cancer, while none of the rest literature had mentioned the diagnostic criteria. There were 11 RCT that have described the stages of breast cancer, in which only 4 RCT adopt UICC or TNM standard. And there were only 7 RCT that had described the types of breast cancer and SI of 14 RCT came from "Limin pharmaceutical factory". The non-unified diagnostic criteria, undefined stages and types, as well as the inconsistent source of administered medicine had affected the meta-analysis results.
Any kind of treatment measures or therapeutics may cause untoward effects in various extents. The monitoring on untoward effects of drug intervention has important significance for guiding clinical medication and evaluating drug efficacy. However, the literature involved in this study has only reported the untoward effects, while it is unclear whether there are untoward effects in the research process of other experiments, indicating that the researchers do not pay sufficient attention to the observation and report of untoward effects. This will be adverse to the application and promotion of SI treatment for breast cancer.
Conclusion
Currently the methodology and reports of clinical research on the combination of shenqi fuzheng and chemotherapy to treat breast cancer are with low quality, and cannot provide scientific and reliable basis for clinical application. So, it suggests following the standard of the multi-center and large-sample randomly controlled double-blind trials to design the experiments rather than the low-level duplicates.
References
Ai Q, Zhang W, Xie Y, Huang W, Liang H, Cao H. Post-marketing safety monitoring of shenqifuzheng injection: A solution made of dangshen (Radix Codonopsis) and huangqi (Radix Astragali Mongolici). J Tradit Chin Med. 2014; 34: 498-503.
Bo Y, Li HS, Qi YC, Lu MY. Clinical study on treatment of mammary cancer by shenqi fuzheng injection in cooperation with chemotherapy. Chin J Integr Med. 2007; 13: 37-40.
Chen F, Lin H. Clinical observation of shenqifuzheng injection in assist chemotherapy of breast cancer. Strait Pharmaceutical J. 2007; 19: 75-76.
Chen JM X X H, L H. Clinical observation of shenqifuzheng injection in the treatment of advanced breast cancer patients with chemotherapy. Mod J Integ Trad Chin West Med. 2010; 19: 2651-52.
Cui YZ, ZSJHYG. Shenqifuzheng injection prevented anthracycline cardiotoxicity. Hebei Med J. 2010: 1685-86.
Dai Zj WXJ. Clinical observation of efficacy and adverse reactions on Shenqifuzheng injection used in patients with breast cancer receiving neoadjuvant chemotherapy. ADRJ. 2010: 10-14.
Deng Y, Chen HF. Effects of Astragalus injection and its ingredients on proliferation and Akt phosphorylation of breast cancer cell lines. Zhong Xi Yi Jie He Xue Bao. 2009; 7: 1174-80.
Horton JK, Siamakpour-Reihani S, Lee CT, Zhou Y, Chen W, Geradts J, Fels DR, Hoang P, Ashcraft KA, Groth J, Kung HN, Dewhirst MW, Chi JT. FAS death receptor: A breast cancer subtype-specific radiation response biomarker and potential therapeutic target. Radiat Res. 2015; 184: 456-69.
Huang ZF, Wei JS, Li HZ. Effect of Shenqi Fuzheng injection combined with chemotherapy on thirty patients with advanced breast cancer. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2008: 28: 152-54.
Kawuli. Curative effect observation: Shenqifuzheng injection in the treatment of advanced breast cancer patients with chemotherapy. Guide China Med. 2010: 885-86.
Lee E, Menon U, Nandy K, Szalacha L, Kviz F, Cho Y, Miller A, Park H. The effect of a couples intervention to increase breast cancer screening among korean americans. Oncol Nurs Forum. 2014; 41: E185-93.
Li C, Yang G, Yu M, Xu Y, Xue N, Nan N, Wang X. Effects of traditional Chinese medicine Shu Gan Jian Pi granules on patients with breast cancer and cancer-related fatigue: Study protocol for a randomized controlled trial. Trials 2015; 16: 192.
Li Xl. Clinical observation of shenqifuzheng injection treated advanced breast cancer patients with chemotherapy. Mod Oncol. 2010: 574-75.
Li YQ. 35 cases of Shenqifuzheng injection treated advanced breast cancer patients with chemotherapy. J Chin Integr Med. 2010: 827.
Lie JY. Shenqifuzheng injection in the treatment of â…£ advanced breast cancer patients influence on the serum CA153 and activity of immune cell with chemotherapy. J Practical Oncol. 2010: 885-86.
Lin SQ, Wei XH, Huang P, Liu YY, Zhao N, Li Q, Pan CS, Hu BH, Chang X, Fan JY, Yang XY, Wang CS, Liu HN, Han JY. QiShenYiQi Pills(R) prevent cardiac ischemia-reperfusion injury via energy modulation. Int J Cardiol. 2013; 168: 967-74.
Lu CY, Chen XY. Progress of research on apoptosis of breast cancer cells. Zhong Xi Yi Jie He Xue Bao. 2003; 1: 226-29.
Lu MY. The effects of shenqifuzheng injection on the immune function of patients with breast cancer treated with CAF regimen chemotherapy. J Basic Clin Oncol. 2010; 23: 236-38.
McCarthy N, Boyle F, Zdenkowski N, Bull J, Leong E, Simpson A, Kannourakis G, Francis PA, Chirgwin J, Abdi E, Gebski V, Veillard AS, Zannino D, Wilcken N, Reaby L, Lindsay DF, Badger HD, Forbes JF. Neoadjuvant chemotherapy with sequential anthracycline-docetaxel with gemcitabine for large operable or locally advanced breast cancer: ANZ 0502 (NeoGem). Breast. 2014; 23: 142-51.
Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche PC, Devereaux PJ, Elbourne D, Egger M, Altman DG. CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. 2010; 63: e1-37.
Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche PC, Devereaux PJ, Elbourne D, Egger M, Altman DG. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. Int J Surg. 2012; 10: 28-55.
Pu Z, Yuan X, Zhang X, Chen Q, Xie H. Meta-analysis on the association between CYP2D6*10 gene polymorphism and disease free survival of breast cancer patients receiving tamoxifen treatment in Asia. Bangladesh J Pharmacol. 2014; 9.
Pu Z, Zhang X, Chen Q, Yuan X, Xie H. Establishment of an expression platform of OATP1B1 388GG and 521CC genetic polymorphism and the therapeutic effect of tamoxifen in MCF-7 cells. Oncol Rep. 2015; 33: 2420-28.
Raia-Barjat T, Trombert B, Khaddage A, Douchet C, Seffert P, Peoc'h M, Falk AT, Magne N, Chauleur C. OSNA (one-step nucleic acid amplification) sentinel lymph node intraoperative molecular analysis in breast cancer: A cost-benefit analysis. Med Oncol. 2014; 31: 322.
Sanchez R, St-Cyr J, Lalonde ME, Healy J, Richer C, Gagne V, Laverdiere C, Silverman LB, Sallan SE, Neuberg D, Kutok JL, Kritikou EA, Krajinovic M, Sinnett D. Impact of promoter polymorphisms in key regulators of the intrinsic apoptosis pathway on the outcome of childhood acute lymphoblastic leukemia. Haematologica 2014; 99: 314-21.
Schmidt T, Weisser B, Durkop J, Jonat W, Van Mackelenbergh M, Rocken C, Mundhenke C. Comparing endurance and resistance training with standard care during chemotherapy for patients with primary breast cancer. Anticancer Res. 2015; 35: 5623-29.
Schulz KF. Assessing allocation concealment and blinding in randomised controlled trials: Why bother? Evid Based Nurs. 2001; 4: 4-6.
Shui Y, Tang Y, Zhang X, Ge J, Pu Z. Adjuvant chemotherapy of megestrol acetate in advanced breast cancer: A meta-analysis. Bangladesh J Pharmacol. 2015; 10: 383.
Sun XZ. Curative effect of shenqifuzheng injection treated advanced breast cancer patients with chemotherapy. J China Trad Chin Med Inform. 2011; 3: 237.
Valadares F, Garbi Novaes MR, Canete R. Effect of Agaricus sylvaticus supplementation on nutritional status and adverse events of chemotherapy of breast cancer: A randomized, placebo-controlled, double-blind clinical trial. Indian J Pharmacol. 2013; 45: 217-22.
von Minckwitz G, Puglisi F, Cortes J, Vrdoljak E, Marschner N, Zielinski C, Villanueva C, Romieu G, Lang I, Ciruelos E, De Laurentiis M, Veyret C, de Ducla S, Freudensprung U, Srock S, Gligorov J. Bevacizumab plus chemotherapy versus chemotherapy alone as second-line treatment for patients with HER2-negative locally recurrent or metastatic breast cancer after first-line treatment with bevacizumab plus chemotherapy (TANIA): An open-label, randomised phase 3 trial. Lancet Oncol. 2014; 15: 1269-78.
Wang SM. The application: Shenqifuzheng injection in the treatment of advanced breast cancer patients with chemotherapy. Med Industry Inform. 2006; 3: 124.
Xiao HW. Shenqi-fuzheng injection combined with FEC in the treatment of breast carcinoma. J Med Theor Prac. 2005; 18: 885-86.
Xie W, Zhao Y, Zhang Y. Traditional chinese medicines in treatment of patients with type 2 diabetes mellitus. Evid Based Complement Alternat Med. 2011; 2011: 723-26.
Xu HJ. Clinical research of Shenqi-fuzheng injection reduced the cardiac toxicity of breast cancer with TA. Chinese community doctors. 2010; 36: 130.
Xu NL. The effects of Shenqifuzheng injection on the immune function of patients with breast cancer treated with chemotherapy. Henan Medical Information. 2003; 24: 12.
Yao K, Ma Y, Ma W, Hu J, Wang C, Chen J, Zhang J, Hua L, Ren X. Shenqifuzheng injection combined with chemotherapy in the treatment of advanced gastric cancer: A systematic review and meta-analysis. J Cancer Res Ther. 2014; 10 Suppl 1: 70-74.
Ye MN, Chen HF. Effects of Astragalus injection on proliferation of basal-like breast cancer cell line MDA-MB-468. Zhong Xi Yi Jie He Xue Bao. 2008; 6: 399-404.
Yuan JW, Kong CB, Kang GQ, Liu XF, Yang SJ. Effects of neoadjuvant chemotherapy combined with shenqifuzheng injection on cell immune function patients with breast cancer. Lishizhen Med Mater Res. 2008; 19: 1099-100.
Ze Y. Shenqifuzheng injection treated advanced breast cancer patients with chemotherapy. Shandong Med J. 2011; 51: 109.
Zhang RL. The role of chemotherapy: Shenqi fuzheng injection on the immune function of patients with breast cancer. J medical forum. 2004; 25: 48.
Zhu K. Clinical observation of shenqi fuzheng injection in the treatment of advanced breast cancer patients with chemotherapy. J Mod Oncol. 2010; 19: 2651-52.
Zou TL. The attenuation of shenqi fuzheng injection treated advanced breast cancer patients with chemotherapy. J Pract Oncol. 2006; 21: 75-77.